Shock
Definition
A serious condition that occurs when the cardio-vascular system is unable to supply enough blood flow to the body, causing inadequate tissue perfusion.
Major classes of shock include:
- Cardiogenic Shock (associated with heart problems)
- Hypovolemic Shock (caused by inadequate fluid volume)
- Anaphylactic Shock (caused by allergic reaction)
- Toxic Shock (associated with infections)
- Neurogenic Shock (caused by damage to the nervous system)
Shock is a life-threatening condition that requires immediate medical treatment. Some degree of shock can accompany any medical emergency. Shock can get worse very rapidly.
Recognition
Depending on the specific cause and type of shock, symptoms may include:
- Anxiety or agitation
- Bluish lips and fingernails
- Chest pain
- Confusion
- Cool, clammy skin
- Decreased or no urine output
- Dizziness or light-headedness
- Faintness
- Low blood pressure (Hypotension)
- Paleness (pallor)
- Profuse sweating, moist skin
- Rapid pulse
- Shallow breathing
- Unconsciousness
- Weakness
- Hyperventilating
- Extended capillary refill time >2secs
Cardiogenic Shock
This occurs when heart muscle damaged, most commonly by a severe myocardial infarction, is not able to pump enough blood to meet the needs of the body. Other causes which can compromise cardiac output are:
- Dysrhythmias such as ventricular tachycardias and bradycardia caused by complete heart block.
- Cardiac tamponade where blood/fluid builds up in the pericardium preventing the ventricles expanding fully. There is little that can be done in the prehospital environment for this condition as the patient will require pericardiocentesis and this procedure is rarely carried out in prehospital care.
Hypovolemic shock
A form of shock. A condition where the heart is unable to supply enough blood to the body because of blood loss, or inadequate blood volume. Clinical symptoms may not present until 10-20% of total whole-blood volume is lost.
Causes and Risks:
Loss of approximately one-fifth or more of the normal blood volume produces hypovolemic shock. The loss can be from any cause, including external bleeding, internal bleeding, or diminished blood volume resulting from excessive loss of other body fluids (such as can occur with diarrhoea, vomiting and burns).
Prevention:
Preventing shock is easier than trying to treat it once it happens. Prompt treatment of the underlying cause will reduce the risk of developing severe shock.
Stages of Hypovolemic Shock
Stage 1
- Up to 15% blood volume loss (750mls)
- Compensated by constriction of vascular bed
- Blood pressure maintained
- Normal respiratory rate
- Pallor of the skin
- Slight anxiety
Stage 2
- 15-30% blood volume loss (750 - 1500mls)
- Cardiac output cannot be maintained by arterial constriction
- Tachycardia
- Increased respiratory rate
- Blood pressure maintained
- Increased diastolic pressure
- Narrow pulse pressure
- Sweating from sympathetic stimulation
- Mildly anxious/Restless
Stage 3
- 30-40% blood volume loss (1500 - 2000mls)
- Systolic BP falls to 100mmHg or less
- Classic signs of hypovolemic shock
- Marked tachycardia >120 bpm
- Marked tachypnoea >30 bpm
- Decreased systolic pressure
- Alteration in mental status (Anxiety, Agitation)
- Sweating with cool, pale skin
Stage 4
- Loss greater than 40% (>2000mls)
- Extreme tachycardia with weak pulse
- Pronounced tachypnoea
- Significantly decreased systolic blood pressure of 70 mmHg or less
- Decreased level of consciousness
- Skin is sweaty, cool, and extremely pale (moribund)
The 4 areas that life threatening haemorrhage can occur
- Chest - Myocardium, great vessels, lung lacerations
- Abdomen - Intra-abdominal injuries
- Pelvis/Thighs - Pelvic and Femur fractures
- Entire body - Look over entire body for external haemorrhage
Management
Treat other injuries, Arrest any major external haemorrhage, Keep patient warm, Raise legs to aid venous return, Continually monitor patient vital signs, Reassurance, Keep nil by mouth, patient position - lying flat or in recovery position, High concentration of O2 A paramedic will gain venous entry with a cannula and commence a fluid challenge as part of his/her management of shock
ASHICE (Consider)
Transport to Hospital - Continually monitor patient vital signs.
Professional Handover
Anaphylactic Shock
Anaphylaxis is a sudden, severe, potentially fatal, systemic allergic reaction that can involve various areas of the body. Symptoms occur within minutes to two hours after contact with the allergy-causing substance, but in rare instances may occur up to four hours later. Minute amounts of allergens may cause a mild to life-threatening reaction.
Common causes of anaphylaxis include:
- Food - Peanuts, tree nuts (walnuts, cashews, etc.), shellfish, fish, milk, and eggs commonly cause anaphylactic reactions
- Medication - Anaphylactic reactions to medication will typically occur within an hour after taking the drug, however reactions may occur several hours later
- Insect stings - The symptoms of anaphylactic reactions to insect stings usually occur within minutes of the sting.
- Latex - Approximately 10 to 17 percent of those employed in the health care occupations have this allergy.
Signs and Symptoms
- An itchy nettlerash (urticaria, hives)
- Faintness and unconsciousness due to very low blood pressure. Unlike an ordinary fainting attack, this does not improve so dramatically on lying down.
- Swelling (angioedema)
- Swelling in the throat, causing difficulty in swallowing or breathing
- Asthma symptoms
- Vomiting
- Cramping tummy pains
- Diarrhoea
- Anxiety
- A tingling feeling in the lips or mouth if the cause was a food such as nuts
- Death due to obstruction to breathing or extreme low blood pressure (anaphylactic shock)
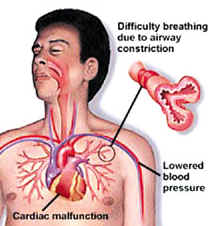
The symptoms are related to the action of immunoglobulin E (IgE) which acts to release histamine and other mediator substances from mast cells. Histamine induces, beside other effects, vasodilation and bronchospasm (constriction of the airways).
Management
Patient position - lying flat with legs raised if comfortable, Consider use of salbutamol for any wheezing, High concentration of O2 Adrenaline 1:1000, Get paramedic backup running, Be prepared to carry out BLS
ASHICE (Consider)
Transport to Hospital
Professional Handover
Neurogenic Shock
A sudden disruption of signals that maintain autonomic nervous system control over vasoconstriction leading to hypotension, occurs after an acute spinal cord injury that blocks sympathetic activity. Neurogenic shock should be suspected if there is a cervical or high thoracic injury with no signs of fluid loss where the following signs and symptoms are exhibited.
Signs and symptoms:
- Hypotension
- Bradycardia
- Warm, dry extremities
More information
- Wikipedia - Hypovolaemia